Midwifery – an essential component of modern maternity care for enhanced fetomaternal outcomes









Jan 31, 2021
Roopa Balan
Final year resident in Obstetrics & Gynaecology
Every woman loves a wonderful birthing experience be it either normal or cesarean birth.
Imagine, how a woman would feel if she is being told of having a grave condition where she can die on table where she is operated upon.
Imagine being sent away from one hospital to another, denying expertise or team in dealing with such an arduous bullet speed surgery.
God only knows how much that woman would have gone through having to travel all the way from vijayawada and roaming hospital to hospital and at last to land at our ER.
She was pregnant the third time, having lost one child already after birth.
She had both babies delivered by c.section.
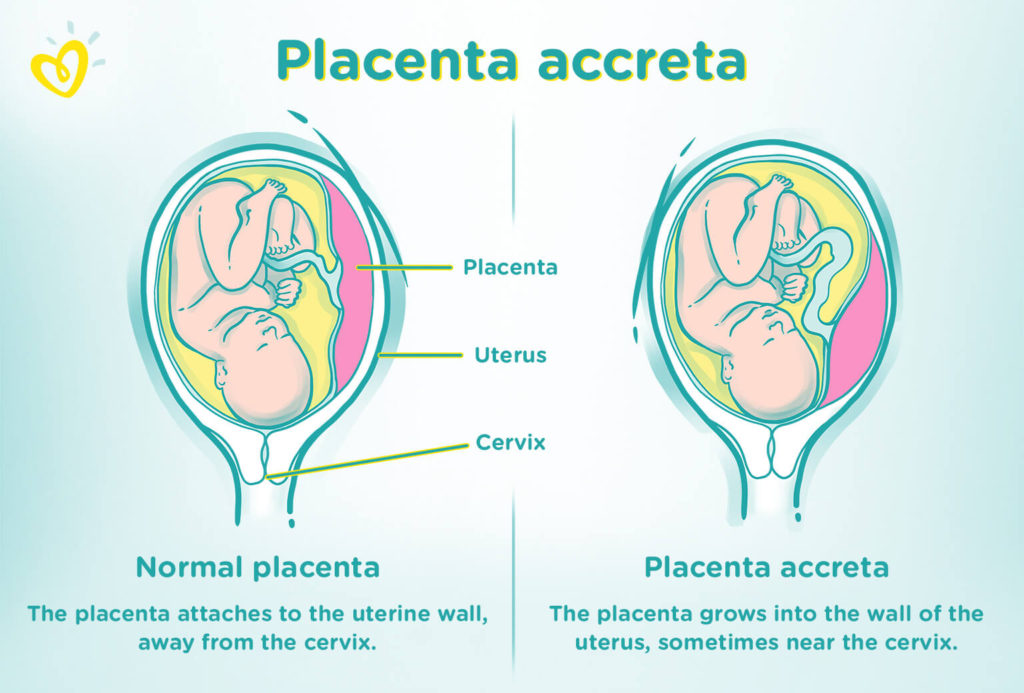
Longing to have one more baby made her land up with a condition called placenta percreta, where the placenta wholly or partially is adherent on the uterus and invading the bladder like a tumour.
Adding to one grave condition, there were 2 other factors making the case even more challenging for any doctor to boldly operate upon her.
She was obese weighing 105kgs and had gestation diabetes mellitus on treatment with insulin.
We admitted her with lots of doubt and even more prayers.
Even a MRI to evaluate the extent of adherence was futile because of being obese.
Mustering all the courage, preparing to operate on her was an exciting experience for all the senior obstetricians and their residents.
Having had a handful of cases operated for the same condition at our facility and with the experience gained, we primed the family every single day to accept anything that might happen.
Then came the day before surgery, where all the junior residents were busy reserving blood for massive transfusion protocol.
I remember the night before where we were awake all night to prepare her.
We where confused whether it was a drill for a military operation or a wedding ceremony.
It was mixed with excitement and terror. Repeating verbatim every resident’s role during surgery , we passed the night.
Urologists , General surgeons , anaesthetists, Pediatricians, radiologists, senior and junior obstetricians, blood bank medical officer, almost 30 or more doctors worked together to save the mother and her baby.
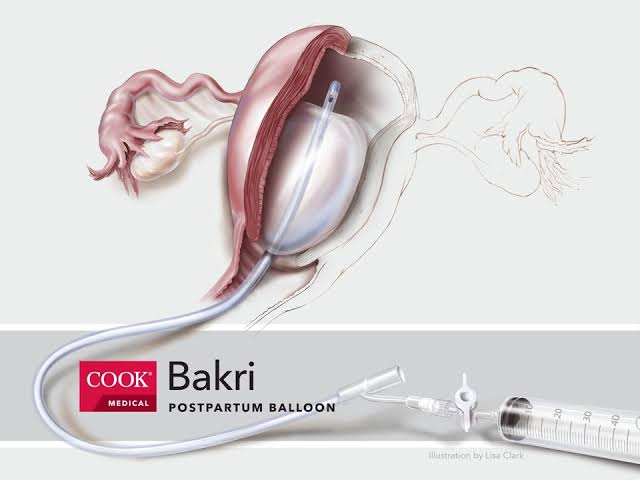
The surgery lasted around 5 hours, having had to remove her uterus, repair her bladder, sending blood after blood, the operation theatre was filled with everyone having their assigned jobs.


Total of 16 products transfused, finally we made it, the patient and her baby made it.
Not everyone make it, we have seen deaths before our eyes, losing young mothers to this grave condition.
We think prevention plays a very important role, limiting family size, avoiding unintended pregnancies and abortions, avoiding c.sections without appropriate indication.
The western countries are more ahead and aware of this condition than us.
We hope awareness spreads in India too.
We hope we prevent deaths and gain more expertise in facing such cases.
Hoping the mother would share her experience very soon after her complete recovery.


Being aware of this complication early in pregnancy and adequate management at a higher center under multi disciplinary team can save lives !!
A 24 hours duty in a tertiary maternity hospital can be nothing short of walking on a tight rope …
On 2 -11-2020 @ 2 P.M they gave me in handover ….
10 P.M …there comes another multi …4th Gravida with 3 Previous Caesreans and draining liquor now , we had to open her with a high risk consent for intraabdominal adhesions ( in view of 3 previous surgeries) , risk of visceral injury , bleeding , hysterectomy , need for blood transfusion and other possible post operative complications. As expected uterus was densely adherent to abdominal wall and we struggled to get access to the uterus , fortunately the surgery went well without any complications .
Few more women who had Previous Caesarean delivery had come in labour , we had to continue doing cases all through the night …no rest , no sleep !
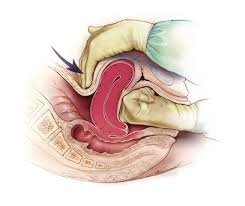
And suddenly there was another PPH , this time traumatic one , because of precipitate labour in a Primigravida , because her labour was induced ! Cervix was explored and a deep tear was found which was sutured . She lost nearly 1500 ml blood and we gave her blood transfusion.
@ 1 A.M All of us exhausted physically and mentally , there was another case of abruption , G3 P1 L0A1 with 24 weeks with Previous Caesarean , referred from Devarakonda with complaints of bleeding per vaginum since 4 hours , clothes soaked in blood, Hb 4.5gm ,we needed to deliver her somehow within 2 hours , because when there is abruption of placenta ( premature separation of placenta before delivery ) , the woman needs to deliver within 6 hours otherwise she will go into shock and DIC , blood coagulation defects can occur ,causing multiple organ failure. I gathered enough courage and gave her Misoprostol 50 micrograms ( she is a case of Previous Caesarean … her risk of uterine rupture needs to be balanced against the risk of surgery at this point of time )
… she fortunately expelled the dead foetus of 24 weeks . She received 2 packed cell transfusion too.
2 A.M in the night ,a G3 P2 L2 with 9 weeks gestation, bleeding profusely , because of incomplete abortion , she was dead pale , Hb 4.2 gm , AB negative blood , not available anywhere in the city in that night , not even O negative could be found in any of the blood banks !
3 A.M : An unbooked woman from Orissa , G3 P2 L0 …no live children, delivery gets complicated because of Shoulder dystocia , baby 3.9 kg 😱
4 A.M …A woman with triplets and 35 weeks comes with draining …, she had a cervical cerclage in situ which was removed .
5 A.M HELLP syndrome Pt with AKI delivers and referral done to Osmania General Hospital as she needs dialysis .
6 A.M More inductions of labour started , as some of the previous inductions end successfully .
7 A.M …A G2 P1L0 with 34 weeks admitted in view of complete placenta praevia ( Type 4 …covering the internal os ) , starts trickling blood and sets into labour …
8:15 A.M ….Another G2 P1 L1 with 39 weeks with previous C – Section comes in labour and we had to post it at 8:45 am
A total of 11 C- Sections , 43 vaginal deliveries , many requiring blood transfusions …
All possible complications of Obstetrics experienced thoroughly …thank God , there were no cases of rupture uterus and rupture ectopic in this duty !!
Child birth is never easy , death can drop in every moment and any moment …
I wonder why people tend to take the whole process for granted …
women’s lives do matter ...
“It took me quite a long time to develop a voice, and now that I have it, I am not going to be silent.” – Madeleine Albright

Mrs . A , 27 yr old woman referred from CHC, Zaheeraabaad to our hospital MGMH, Petlaburz, Hyderabad on 23.09.2020 at 4:30 a.m in view of G2 P1L1 with 1 previous LSCS with term gestation, severe preeclampsia and thrombocytopenia of 84,000.
on reaching here , she had a convulsion , her BP was 160/110 .PR 86/min . She was started on MgSO4 regimen .She had extensive pedal oedema Obstetric examination revealed a term gestation per abdomen ,a constriction-ring at the level of umbilicus , the part of uterus above the umbilicus deviated to right ,part below the umbilicus moved to left and it had a boggy feel , per vaginum Cervix effaced and Os dilated to 3 cm , presenting part brow .
USG examination confirmed a rupture uterus with a live foetus .she was taken up for immediate laparotomy . A general anaesthesia was given . Intraoperative findings were consistent with the scan findings . The previous scar had given away along with the bladder that was adherent to it .A live male foetus 2.5 kg was delivered by Patwardhan technique . The lower flap of the uterine scar could not be identified as the entire tissue was oedematous . Bladder integrity checked by retrograde filling . The rent in the bladder dome was identified and urologist called for . The bladder was adherent on the posterior surface to the lower segment, which was dissected and bladder repaired in 2 layers . Uterus lower segmented inspected for extension of any tears , colporrhexis was ruled out and uterine scar sutured . A suprapubic catheter , per urethral catheter and abdominal drain were kept .She was stable throughout the procedure, received 2 packed cell transfusions intra- operatively .MgSO4 regimen continued for 24 hours and thromboprophylaxis , Piptaz cover were given .she is doing well now and happy with her baby .